What is the TEAM
In April of this year, the Centers for Medicare & Medicaid Services (CMS) announced a proposed update to the FY 2025 Hospital Inpatient Prospective Payment System (IPPS) and Long-Term Care Hospital Prospective Payment System (LTCH PPS) Proposed Rule (CMS-1808-P). Among the updates related to this measure, this blog will focus on the new standout mandatory 5-year, episode-based alternative payment model (APM) called TEAM—short for the Transforming Episode Accountability Model.

Background & Important Dates Regarding Current Payment Models and Transforming Episode Accountability Model (TEAM)
CMS has developed, evaluated and tested over 50 APMs since its inception in 2010, but TEAM is the first mandatory model across five surgical procedures. APM models like TEAM reward healthcare providers for effectively delivering value-based care by testing different healthcare service delivery approaches and payment models. Continuing the shift away from traditional fee-for-service (FFS) reimbursement to value-based care, there is a continued focus on quality of care instead of the quantity.
Historically, the majority of payment models have been voluntary. CMS has shared in their frequently asked questions document that they have learned from past voluntary models and want to conduct advanced testing and evaluation of financial accountability for episode-based care as an approach to improve quality of care for patients and lower costs. In the response document, CMS finds that, “Mandatory models can improve the generalizability of model findings and capture a wider variety of providers across the country…it also addresses participation challenges inherent to voluntary models – namely provider attrition and selection bias.”
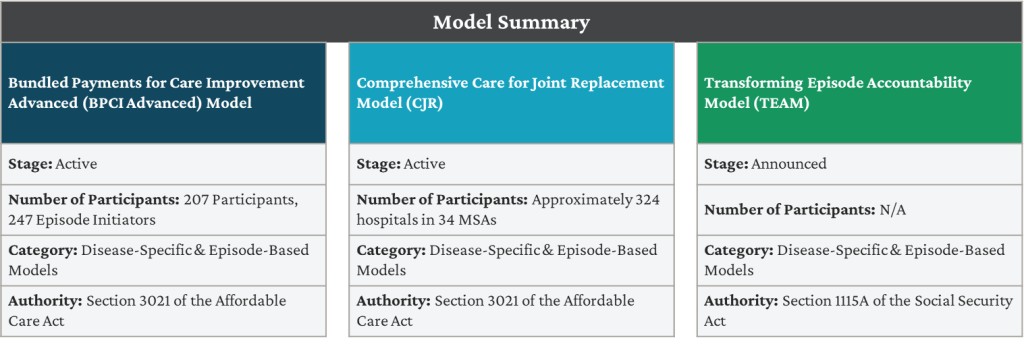
TEAM currently overlaps with both CJR and the Bundled Payments for Care Improvement Advanced (BPCI Advanced). CJR is set to expire December of 2024, and BPCI Advanced is anticipated to end December of 2025. As a refresher, let’s look at these models side by side.
BPCI Advanced: The model is part of the continuing efforts by CMS and Center for Medicare and Medicaid Innovation (Innovation Center) in implementing voluntary episode payment models. It aims to support healthcare providers who invest in practice innovation and care redesign to better coordinate care and reduce expenditures, while improving the quality of care for Medicare beneficiaries. BPCI Advanced qualifies as an APM under the Quality Payment Program (QPP).
CJR: The model is designed to improve care for Medicare patients undergoing lower-extremity joint replacement (LEJR) procedures, specifically hip, knee, and ankle replacements. By providing participating hospitals with bundled payments for these procedures, the CJR model encourages hospitals, physicians, and post-acute care providers to work together to improve the quality and coordination of care from the initial hospitalization or outpatient procedure through recovery.
TEAM: Under TEAM, selected acute care hospitals would coordinate care for people with traditional Medicare who undergo one of the surgical procedures included in the model. These hospitals would assume responsibility for the cost and quality of care from surgery through the first 30 days after the Medicare beneficiary leaves the hospital. CMS proposed it would choose acute care hospitals based on inclusion in core-based statistical areas (CBSAs) and pull a random sampling to select approximately 25% of eligible CBSA’s (ineligible include Maryland sites and sites with no episodes in 5 categories).Currently CMS has identified 803 eligible CBSA’s – meaning 200 would be selected for the model.


Sources | BPCI Sources | BPCI Advanced | CMS | bpcia-my6-model-ovw-fs.pdf (cms.gov) | CJR | CMS Comprehensive Care for Joint Replacement (CJR) | TEAMS | Transforming Episode Accountability Model (TEAM) | CMS | team-model-fs.pdf (cms.gov) | CMMI Proposes New Mandatory Episode-Based Payment Model – McDermott+Consulting

Episodes, Beneficiary Inclusion Criteria, & Quality Measure & Reporting
Episodes
TEAM focuses onfive surgical procedures: lower extremity joint replacement, surgical hip femur fracture treatment, spinal fusion, coronary artery bypass graft, and major bowel procedure. Each episode begins with an inpatient stay or outpatient procedure related to one of these surgeries.

Beneficiary/Patient Inclusion Criteria
Beneficiary/Patient Inclusion Criteria – must meet the following for admission:
- Enrolled in Medicare Part A and Part B
- Not eligible due to end-stage renal disease
- Not in any managed care plan (e.g., Medicare Advantage)
- Not covered by the United Mine Workers of America health plan
- Medicare as their primary payer
Quality Measures and Reporting
Quality Measures and Reporting – Assessment and eligibility for TEAM payments rely on measures reported through the Hospital Quality Reporting Program (IQR) program:
All TEAM episodes:
- Hybrid Hospital-Wide All-Cause Readmission Measure
- CMS Patient Safety and Adverse Events Composite
LEJR Episodes (TKA/THA Focus):
- Hospital-Level Total Hip and/or Total Knee Arthroplasty (THA/TKA) Patient Reported Outcome-Based Performance Measure (PRO-PM)
Participation and Financial Tracks & Methodology
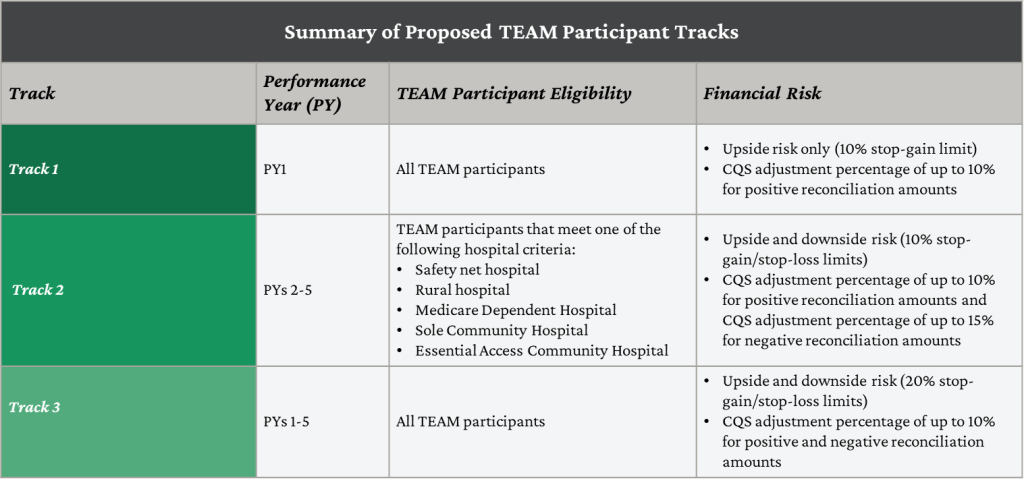
TEAM prioritizes health equity by offering flexibilities to hospitals that serve underserved populations. These flexibilities, or tracks, reduce the financial burden associated with value-based model participation.

Source | CMS TEAM Fact Sheet
Hospitals that choose Tack 1 would have no downside risk and lower levels of reward for the first year. Track 2 would be associated with lower levels of both risk and reward for certain hospitals (see diagram below), such as safety net hospitals, for years 2 through 5. Track 3 would be associated with higher levels of risk and reward for years 1 through 5. TEAM participants would be required to notify CMS of their track selection prior to the start of PY 1. If participants do not self-select, CMS will automatically assign them to Track 1 for PY 1. If TEAM participants select Track 1 for PY 1, they would be automatically assigned to Track 3 for PY 2-5. One track’s target pricing methodology includes a social risk adjustment to account for the additional investment needed to care for underserved individuals. Participating hospitals submit health equity plans and sociodemographic data to CMS, while also screening individuals for health-related social needs.
CMS proposes using three years of baseline data, projected to the performance year, to calculate target prices at the level of MS-DRG/HCPCS episode type and region.These episode-level target prices would be risk-adjusted, aligning with the approach used in PYs 4–8 of the CJR model. Additionally, CMS suggests applying a 3% discount factor to the benchmark price, representing Medicare’s share of reduced expenditures from the episode
Also, CMS plans to conduct an annual reconciliation process. During this reconciliation, CMS would compare spending for a TEAM participant’s beneficiaries in episodes against the reconciliation target price. If the actual spending exceeds the target, the participant may owe CMS a repayment, while if it falls below, CMS may owe the participant a reconciliation payment. The reconciliation occurs six months after the end of the performance year.
Closing Summary
The goal of the Transforming Episode Accountability Model (TEAM) measure, as proposed by CMS, is to improve the quality and cost-effectiveness of care for Medicare beneficiaries. It introduces a mandatory five-year episode-based payment model, where selected hospitals are held accountable for the total cost and quality of care during and 30 days after certain surgical procedures. TEAMS aims to incentivize care coordination, enhance patient care transitions, and reduce avoidable readmissions. The model includes a social risk-adjustment to account for the care of underserved individuals and offers tracks with varying financial risks and rewards. Hospitals will be evaluated based on their spending against target prices and performance on quality measures. The measure is designed to shift from fee-for-service to value-based care, emphasizing quality over quantity. It is set to begin on January 1, 2026, and will run until December 31, 2030. TEAMS represents CMS’s continued efforts to test healthcare service delivery and payment models that reward value-based care.
Stay Ahead Of CMS’ Transforming Episode Accountability Model (TEAM)
Gain a deeper understanding of the TEAM and its impact on your hospital’s surgical care strategy. Our guide covers everything you need to know, from specific procedure codes to reporting timelines, helping you navigate this important shift with confidence.





