Background
The purpose of this blog is to offer healthcare leaders and providers an overview of the TEAM model recently finalized in the FY2025 Inpatient Prospective Payment System (IPPS) final regulation. For background, our previous blog, “TEAMing Up For Better Care: CMS’ Newest Payment Model Impacting IPPS,” provides a comprehensive comparison of the Comprehensive Care for Joint Replacement (CJR) and Bundled Payments for Care Improvement (BPCI) models. These models have laid the groundwork for the new Transforming Episode Accountability Model (TEAM). The blog was based on the proposed TEAM model and was written before nearly 6,000 public comments were collected.
The Centers for Medicare & Medicaid Services (CMS) recently unveiled the FY 2025 Inpatient Prospective Payment System (IPPS) final regulation, which estimates that testing the TEAM model will save the Medicare program $481 million over the five performance years (CMS FY 2025 IPPS Final Rule, p26). The TEAM model aims to address fragmented and costly care for Medicare beneficiaries by enhancing care coordination and health outcomes. If successful, the model could establish “managing episodes as a standard practice in Traditional Medicare” (CMS FY 2025 IPPS Final Rule, p1750). CMS has indicated that it will review and refine policies in the future with notices. However, the industry has much to prepare for as the model starts on January 1st, 2026, and ends on December 30th, 2030.
Impact on Orthopedic and Specialty Surgery
The TEAM model is expected to impact in the orthopedic and specialty surgical spaces. A key change is making it mandatory and directly linking reimbursement to quality measures reported by patients through Patient-Reported Outcomes (PROs). As a result, the prioritization of both the collection of adequate data and the delivery of high-quality care will be more important now than ever.
A step further, the TEAM model encompasses a wider range of episodes beyond lower extremity joint replacement (LEJR), such as surgical hip/femur fracture treatment (SHFFT), spinal fusion, coronary artery bypass graft (CABG), and major bowel procedures. This expansion will necessitate adjustments to new types of procedures and patient care standards.
Final Episodes

Source: CMS 2025 IPPS Final Rule, p1926
Practices with prior experience in mandatory alternative payment models and effective quality reporting are likely to find the transition to TEAM more manageable. However, those unfamiliar with these requirements will need to invest in their people, processes, and technologies to meet the new standards. Overall, the TEAM model seeks to promote a more integrated and patient-centered approach to care, potentially leading to improved outcomes and cost savings in the field.
Standardizing Definitions & Reviewing Key Updates to the TEAM Framework
The Transforming Episode Accountability Model (TEAM) is a mandatory episode-based alternative payment model, in which selected acute care hospitals will coordinate care for people with Traditional Medicare undergoing specific surgical procedures included in the model (initiate an episode), and assume responsibility for the cost and quality of care from surgery through the first 30 days (differs from BPCI and CJR which are 90-day episodes) after the Medicare beneficiary leaves the hospital.
Defining a Medicare Beneficiary
TEAM beneficiaries include Medicare beneficiaries who, at the time of admission to anchor hospitalization or anchor procedure, meet all of the following criteria:
- Enrolled in Medicare Part A and Part B
- Not eligible for Medicare based on end-stage renal disease
- Not enrolled in any managed care plan
- Not covered under a United Mine Workers of America health plan
- Have Medicare as their primary payer
Source: CMS FY 2025 IPPS Final Rule, p2594
TEAM Participants
TEAM participants are defined as acute care hospitals that initiate episodes and are paid under the IPPS with a CMS Certification Number (CCN) primary address located in one of the mandatory CBSAs (CMS FY 2025 IPPS Final Rule, p1768).
Core-Based Statistical Areas Identified: CMS used Core-Based Statistical Areas (CBSAs) to identify selected geographic regions for the model test. Hospitals paid under the Inpatient Prospective Payment System (IPPS) and located in the selected CBSAs are required to participate in TEAM. The list of selected mandatory CBSAs are published in the final rule (See TABLE X.A.-07: LIST OF MANDATORY CBSAs SELECTED FOR PARTICIPATION IN TEAM – Starting on p1885 of Final Reg)
An update in the final regulations states that CMS will also allow a one-time voluntary opt-in opportunity for hospitals participating until the last day of the last performance period in the BPCI Advanced model, or the last day of the last performance year in in the CJR model – which are December 31, 2025, and December 31, 2024, respectively. Eligible hospitals interested in voluntary opt-in will be required to submit a written participation election letter to CMS in a form and manner specified by CMS during the voluntary election period of January 1, 2025-January 31, 2025.
Includes:
- Safety-net hospitals
- Rural hospitals
- Medicare Dependent Hospitals
- Sole Community Hospitals
- Essential Access Community Hospitals
Performance Period
Under the TEAM framework, CMS introduced performance years specific to this bundled payment model. Since TEAM includes multiple reporting years, the performance year more accurately defines the periods during which the model is active. There are five distinct Performance Years (PY) under TEAM. (CMS FY 2025 IPPS Final Rule, p1103-1105)
Definitions
CQS: Composite Quality Score
CQS Adjustment Percentage: The rate applied by CMS to the positive or negative reconciliation amount, based on the TEAM participant’s CQS performance. Hospitals need a CQS of 100 to receive the highest quality-adjusted reconciliation amount.
CQS Adjustment Amount: The value deducted from the positive or negative reconciliation amount to determine the final payment or repayment amount. (CMS FY 2025 IPPS Final Rule, p2117)
Final TEAM Participation Tracks
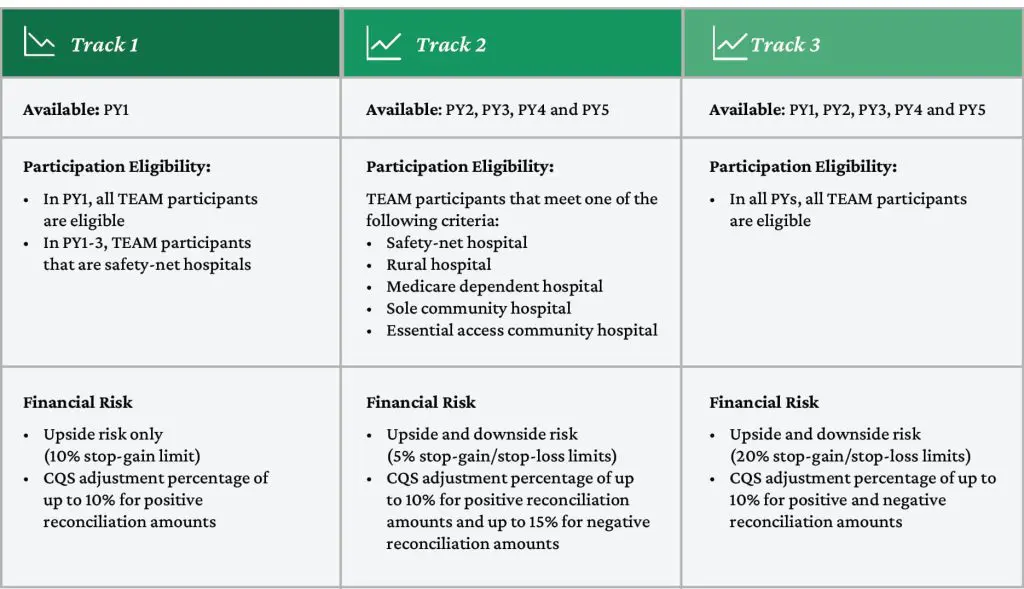
Sources | (CMS FY 2025 IPPS Final Rule, p1822)
CMS states TEAM participants would be fully financially responsible for the episode, though the hospital can make financial arrangements with other providers. They introduced three participation tracks to ease into risk:
- Track 1: Available only in the first PY for all TEAM participants, offering only upside financial benefit (up to 10% of the target price) with a quality adjustment to positive reconciliation amounts.
- Track 2: Available in PYs 2 through 5 for a limited set of TEAM participants, including safety net hospitals, with two-sided financial risk (up to 10% stop-gain/stop-loss limits) and a quality adjustment to reconciliation amounts.
- Track 3: Available in PYs 1 through 5 for all TEAM participants , with two-sided financial risk (up to 20% stop-gain/stop-loss limits) and a quality adjustment to reconciliation amounts.
In the final regulation, CMS revised the risk tracks, allowing safety net hospitals to stay in the upside-only track for PYs 1 to 3. For certain TEAM participants (safety net hospitals, rural hospitals, Medicare-dependent hospitals, sole community hospitals, and essential access community hospitals), CMMI reduced the upside and downside risk options from 10% to 5% stop-gain/stop-loss limits for PYs 2 through 4.
Excluded from TEAM: Hospitals in Maryland, which are not paid under IPPS, as well as hospitals where no TEAM episodes were initiated (CMS FY 2025 IPPS Final Rule, p1770).
AHEAD Model: Despite feedback during the comment period, hospitals in the AHEAD model are not excluded from TEAM.
Sharing Agreements: CMS will permit participating hospitals to establish sharing arrangements with other providers. Essentially, to succeed in the model, hospitals can collaborate with other providers and agree to distribute any reconciliation payments among them (CMS FY 2025 IPPS Final Rule, p2224).

Understanding Episode Timelines in the TEAM Framework
Episodes under the TEAM framework can begin in one of two ways (CMS FY 2025 IPPS Final Rule, p22):
- Anchor Hospitalization: This refers to an admission to an acute care hospital.
- Anchor Procedure: This involves an outpatient procedure at a hospital outpatient department.
The 30-day period starts on the day of admission or the day of the procedure, unless the admission occurs on the same day as the procedure for the same episode category, or the admission happens within three days of the procedure for the same episode category. In these cases, the 30-day period starts from the date of the procedure.
Episodes may include multiple hospitalizations due to readmissions or transfers. If more than one hospitalization occurs within a single episode, CMS will hold the hospital where the episode was initiated as the accountable site.
Episodes end 30 days after the hospital discharge or anchor procedure.
Items and Services Included
The TEAM framework aims to promote comprehensive, coordinated, and patient-centered care through inclusive episodes. It proposes to include all items and services paid under Medicare Part A and Part B during the performance period, except for specific exclusions. This includes the range of services below (CMS FY 2025 IPPS Final Rule, p1926 & p1927):
- Physician Services
- Inpatient hospital services, including those paid through IPPS operation and capital payments
- Inpatient psychiatric facility services
- Long-term care hospital services
- Inpatient rehabilitation facility services
- Skilled nursing facility services
- Home health agency services
- Hospital outpatient services
- Outpatient therapy services
- Clinical laboratory services
- Durable medical equipment
- Part B drugs and biologicals, except those excluded
- Hospice services
- Part B professional claims dated in the 3 days prior to anchor hospitalization if a claim for the surgical procedure for the same episode category is not detected as part of the hospitalization because the procedure was performed by the TEAM participant on an outpatient basis, but the patient was subsequently admitted as an inpatient
TEAM Quality Measures
Impact of Quality Measures on TEAM Reconciliation
Under the TEAM program, participant performance on quality measures will influence their composite quality score (CQS), which in turn directly affects payment reconciliation at the end of each performance year. This effectively ties quality performance to reimbursement.
To minimize reporting burdens, CMS has chosen to use quality measures already included in the Hospital Inpatient Quality Reporting (IQR) and Hospital-Acquired Condition (HAC) Reduction programs:
- For all TEAM episodes:
- Hybrid Hospital-Wide All-Cause Readmission (HWR) Measure with Claims and Electronic Health Record Data
- CMS Patient Safety and Adverse Events Composite (PSI 90)
- For LEJR episodes (Inpatient):
Submission Requirements for Quality Measures
Hospitals are required to submit the Hybrid HWR and THA/TKA PRO-PM measures in the same manner as they do under the IQR program, adhering to the same performance period and submission schedule. The PSI 90 measure, on the other hand, follows the performance period of the HAC Reduction Program.

Source: (CMS FY 2025 IPPS Final Rule, p2003)
Annual Reconciliation
CMS will conduct reconciliation annually, six months after the end of each performance year (CMS FY 2025 IPPS Final Rule, p2035 & p2099).
- Adjustment for Quality: The TEAM participant reconciliation amount, which is the fee-for-service (FFS) expenditure relative to the “target” price, is adjusted based on CQS. The CQS is calculated based on performance on the finalized quality measures.
- Volume-Weighted Quality Measures: Since not all quality measures apply to all episode categories, CMS will weight quality measures that apply to more episode categories more heavily in the CQS. This is done by normalizing the weight as the volume of the episode category divided by the total episode volume.
- Calculation of CQS: The normalized weights are then multiplied by the scaled quality measure scores to produce weighted scaled scores. These scores are combined to produce the final CQS.
Evaluation of the Model: CMS will conduct thorough evaluations of all models it tests. For the TEAM model, CMS has finalized the design and evaluation methods, data collection strategies, key research questions, and the evaluation period, along with anticipated reports. This structured approach ensures that the reconciliation process is fair and reflective of the quality of care provided.
Finalization of Key Features of the TEAM Model
Referral to Primary Care: TEAM participants are now required to include a referral to a primary care provider in their hospital discharge planning for TEAM beneficiaries. This referral must be made on or before discharge from an anchor hospitalization or procedure (CMS FY 2025 IPPS Final Rule, p2351).
Data Sharing: CMS will provide TEAM participants with access to certain beneficiary-identifiable claims data and regional aggregate data, enhancing transparency and data-driven decision-making.
Voluntary Decarbonization and Resilience Initiative: This initiative aims to help hospitals address the health threats posed by climate change. It includes technical assistance for all interested TEAM participants and a voluntary reporting option to capture information on reducing greenhouse gas emissions and improving patient outcomes (CMS FY 2025 IPPS Final Rule, p2380 & 2445).
Conclusion
The introduction of the Transforming Episode Accountability Model (TEAM) marks a significant development in Medicare’s approach to care coordination and cost management. By incorporating insights from previous models like CJR and BPCI, TEAM aims to improve the efficiency and effectiveness of healthcare delivery for Medicare beneficiaries.
This model’s emphasis on mandatory participation ensures widespread adoption, while its performance-based tracks incentivize providers to achieve higher standards of care. Additionally, the incorporation of quality measures highlights CMS’s dedication to not only reducing costs but also improving patient outcomes.
As the healthcare industry gears up for the implementation of TEAM, providers will be encouraged to collaborate more closely, leading to more cohesive and patient-centered care. The focus on quality measures, including PRO-PM, ensures that patient care remains at the forefront of these efforts, with the goal of achieving better health outcomes.
Stay Ahead Of CMS’ Transforming Episode Accountability Model (TEAM)
Gain a deeper understanding of the TEAM and its impact on your hospital’s surgical care strategy. Our guide covers everything you need to know, from specific procedure codes to reporting timelines, helping you navigate this important shift with confidence.




