How Does BMI Affect Outcomes for Total Joint Replacements?
Moving from Complications into Functional Outcomes
Here at CODE, we have been keeping an eye on the growing body of research taking a closer look at the implications of utilizing BMI thresholds for joint replacement eligibility.
With studies transitioning away from the established consensus on BMI vs complication rates and toward BMI vs long term functional outcomes (Roth, et al., 2020; Evans, et al., 2021; Burke et al., 2020 to name a few) – we knew we had to jump in and see how our data registry would weigh in on the matter.
Thomas Fehring, MD was featured in a 2019 article by Benjamin Ricciardi, MD, and indicated that surgeons should focus on three sources of information to continue to monitor and actively advocate for patients with higher BMI. Those sources are big data registries, meta-analyses, and specialty society position statements. Well, we’re in luck! Our CODE registry holds thousands of patients’ long-term Patient-Reported Outcomes (PROs) as well as their biometric data.
We ran reports on function improvement, patient satisfaction, and complication rates based on BMI ranges, and this blog reveals our findings. We know providers are making tough decisions on a daily basis in this arena, and we are always excited to put our data to good use in supporting clinical decision-making.
Quick Summary of Our Findings
Functional Improvement– both TKA and THA patients with a BMI >40 have the greatest improvement in functional outcome scores.
Patient Satisfaction– THA patients with a BMI >40 have the highest level of overall satisfaction. The opposite is true for TKAs- patients with BMI’s >40 report much lower satisfaction rates.
Complications that require additional surgery- patients in the >40 BMI cohort have higher complication rates for both TKA and THA, and there is a stark and drastic increase in the THA >40 group (10.8%, yikes!)
Analysis
For both Total Knee Replacements and Total Hip Replacements, initial review of the CODE registry data aligns with the latest research. Excluding patients who did not participate in the PRO assessment at all intervals, we found that pre-op to post-op functional improvement, captured by the KOOS JR and HOOS JR, was greatest for patients with a BMI >40. This is true across all post-op timepoints up to 3 years and passed analysis for statistical significance.

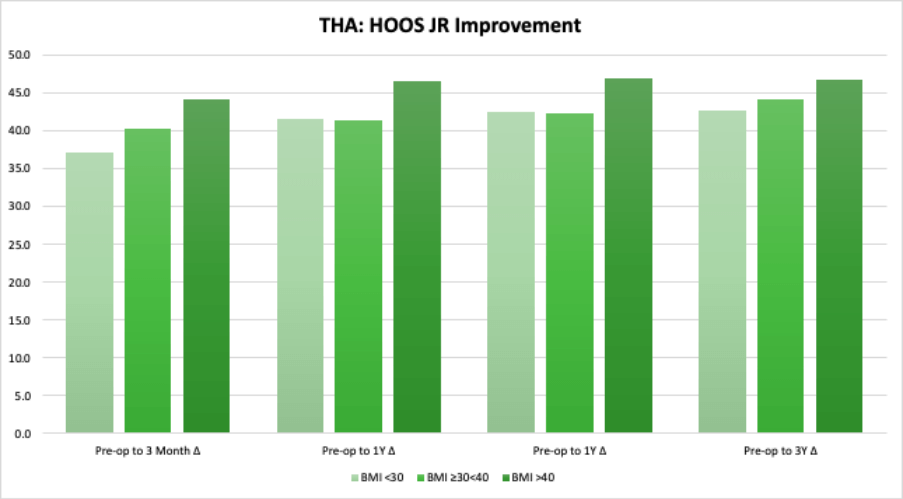
Within the THA population, satisfaction scores for patients with a BMI >40 also exceed those of lower BMI ranges across all timepoints. An impressive 95.9% of THA patients with BMI >40 reported that the results of the surgery had met their expectations at the one year mark.
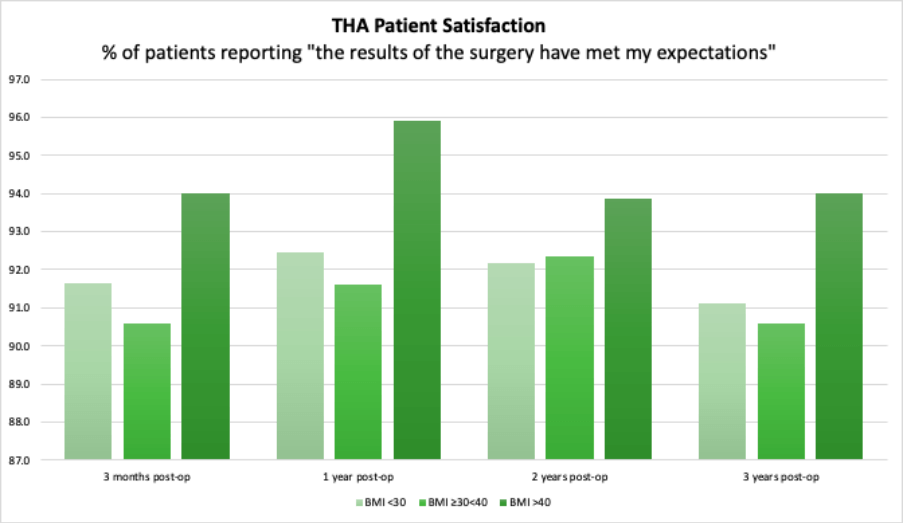
Unfortunately, the same cannot be said for TKA patients, as the >40 BMI group consistently reported lower satisfaction across all timepoints than patients in lower BMI ranges. It would be fair to assume that the intensity of the recovery process likely played a role in that as patient satisfaction scores are significantly lower across all BMI ranges after TKA compared to THA.

Risk-Benefit Shared Decision Making
As mentioned earlier, there is plenty of evidence indicating a higher rate of complications in patients with obesity. Again, our data lines up with past literature; patients with a higher BMI are definitely at increased risk of complications. We found that for TKA patients with a BMI >40 the rate of complications requiring an additional procedure was 3.7% at 3 months compared to 2.07% for patients with a BMI <30, and 1.99% for patients with a BMI between 30-40. For THA patients, the differential is a bit more stark: 10.4% of patients with a BMI >40 reported a complication requiring additional surgery at 3 months, compared to 1.9% of patients with a BMI <30 and 1.6% of patients with a BMI between 30-40. Clearly, the risk of complications is still there, but as the volume of data supporting the magnitude of functional benefits grows, the benefit to risk ratio is prime for surgeon-patient shared decision making.
There’s More to the Value-Based Story
As advocates for value-based care, we can not go without mentioning the fact that this analysis does not take cost into account. While patients across all BMI ranges discussed here clearly hold the potential for life-changing functional improvement, further investigation into the resources required would go hand-in-hand with analysis of complication root cause. It is our opinion here at CODE that complication risk at these rates should not serve to scare providers, but rather it gives us reason to think strategically about how we can better care for these patients.
Perhaps optimization is not about weight loss but about helping the patient to plan ahead; shifting the extra time spent with these patients to the pre-op space vs post-op.
As the body of research grows, we do not see clear evidence to restrict surgery based on a specific BMI threshold. We see an opportunity to utilize PROs and biometric data in shared decision-making between providers and patients and the need to support practices and providers in efficiently anticipating and meeting the needs of these patients.
Download the BMI Report
At CODE, we live for new and exciting ways to make your data actionable. If you found this report at all helpful, feel free to download it and keep it forever!
or Schedule a Call with a CODE PRO Expert
References
Burke, DT, Burke D, Al-Adawi, S, Bell, RB, McCargo, T, Panchatcharam, SM. (2020). The effect of body mass index on the functional outcome of patients with hip replacement. The Journal of the International Society of Physical and Rehabilitation Medicine. 3;4:116-120.
Evans, JT, Mouchti, S, William Blom, A, Wikinson, JM, Whitehouse, MR, Beswick, A, Judge A. (July 16,2021). Obesity and revision surgery, mortality, and patient-reported outcomes after primary knee replacement surgery in the National Joint Registry: A UK cohort study. PLOS Medicine.
Ricciardi, BF, Giori, NJ, Fehring, TK. (October 28, 2019). Clinical Faceoff: Should Orthopaedic Surgeons Have Strict BMI Cuttoffs for Performing Primary TKA and TKA? Clinical Orthopaedics and Related Research. 477(12): 2629-2634.
Roth, A, Anis, HK, Emara, AK, Klika, AK, Barsoum, WK, Bloomfield, MR, Brooks, PJ, Higuera, CA, Kamath, AF, Krebs, VE, Mesko, NW, Murray, TG, Muschler, GF, Nickodem, RJ, Patel, PD, Schaffer, JL, Stearns, KL, Strnad, G, W, JA, Zajichek, A, Mont, MA, Molloy, RM, PIuzzi, NS